3 Questions: Omar Abudayyeh and Jonathan Gootenberg on COVID-19 tests
Two CRISPR scientists explain how COVID-19 tests work, why they're in short supply, and how a CRISPR tool may help solve the problem.
One key to stopping the spread of COVID-19 is knowing who has it. A delay in reliable tests and COVID-19 diagnostics in the US has unfortunately painted an unreliable picture of just how many people are infected and how the epidemic is evolving. But new testing options are now becoming available and the information from these diagnostics will help guide decisions and actions important for public health.
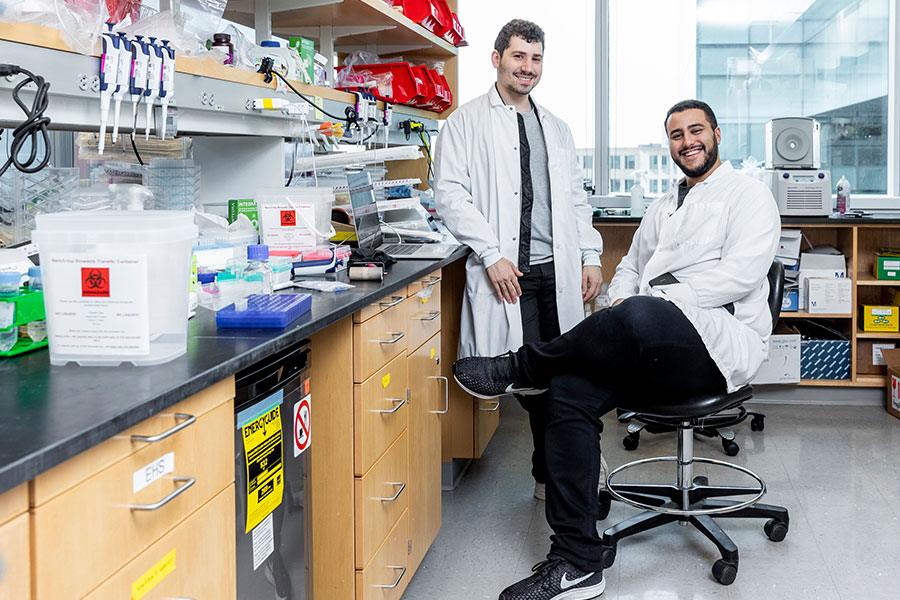
To find out more about the current state of COVID-19 testing, we contacted McGovern Institute Fellows, Omar Abuddayeh and Jonathan Gootenberg, who have been developing CRISPR technologies to rapidly diagnose COVID-19 and other infectious diseases.
Q: How do COVID-19 tests work?
A. There are three main types of tests:
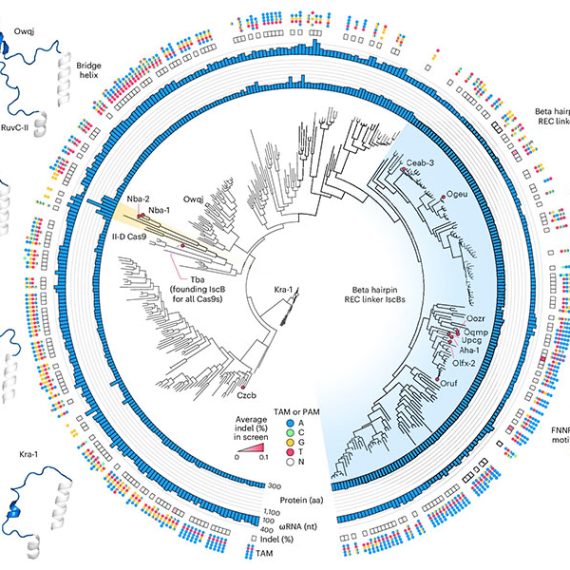
1) Detection of nucleic acid. These tests directly test for the RNA genome of the virus in a variety of sample types, such as nasopharyngeal swabs or sputum. These tests are most commonly performed using polymerase chain reaction (PCR), which can amplify a small part of the virus RNA sequence billions of fold higher to allow detection with a fluorescence measuring instrument. These types of tests are highly sensitive, allowing for early detection of the virus days after infection. PCR tests require complex instrumentation and are usually performed by skilled personnel in an advanced laboratory setting. An alternative method is SHERLOCK, a nucleic acid based test that does not need complex instrumentation and can be read out using a paper strip akin to a pregnancy test, without any loss of sensitivity or specificity. The test is also low cost and can be performed in less than an hour. Because of these features, we are hoping to gain FDA approval that allows deployment at the point of care or at home testing with our COVID-19 SHERLOCK test kit.
2) Detection of viral proteins. Some tests use a paper strip that have antibodies against COVID-19 proteins. These allow for easy detection of the virus in less than an hour but are at least a million-fold less sensitive than nucleic acid based tests because there is no amplification step. This makes them less ideal for screening purposes as many patients will not have enough viral load in sputum or swabs and will receive false negative results.
3) Serology tests detecting antibodies against the virus. These tests can also be used as a paper strip with antibodies that detect other antibodies that develop in someone’s blood in response to COVID-19 infection. Antibodies do not show up in blood until 1-2 weeks after symptoms present, so these tests are not great for catching infection at early stages. Serology tests are more useful for determining if someone has had the infection, recovered, and developed immunity. They may serve a purpose for finding immune people and deciding whether they can go back to work, or for developing antibody-based therapies.
Q. Why aren’t there more COVID-19 tests available?
A. The difficulties in getting nucleic acid detection tests stem from a confluence of multiple factors, including limited supplies of tests, limited supplies of other consumables needed for testing (such as nasal swabs or RNA purification kits), insufficient testing bandwidth at sites that can perform tests (often due to bottlenecks in labor or instruments), and complications behind the logistics of assigning tests or reporting back results. Therefore, just producing more testing material would not solve the issue outright, and either more instrumentation and labor is required, or newer, more rapid tests need to be developed that can be performed in a more distributed manner with reduced dependence on equipment, centralized labs, or RNA purification kits.
Q. What kind of COVID-19 test are you developing now?
A. We are working on a nucleic acid-based test that does not require complex instrumentation, rapidly returns results (with a goal of under one hour), and can be performed at a point-of-care location without trained professionals. We hope to accomplish this using a combination of techniques. First we are incorporating isothermal amplification technologies, which, unlike current PCR-based tests, do not require intricate heating and cooling to operate. We are combining this with our CRISPR-based diagnostics, allowing for sensitive detection and readout in a simple visual format, akin to a pregnancy test. We hope that this test will significantly lower the barrier for accurate diagnosis and provide another approach for COVID-19 surveillance.