Adults’ brain activity appears unchanged after a year of medical use of cannabis
A brain imaging study showed no changes in brain activity during tasks that called on working memory, inhibitory control, or reward processing.
In a study of adults who use cannabis because they are seeking relief from pain, depression, anxiety, or insomnia, scientists at MIT and Harvard found no changes in brain activity after one year of self-directed use. The study, reported September 18, 2024, in JAMA Network Open, is among the first to investigate how the real-world ways people use cannabis to treat medical symptoms might impact the brain in lasting ways.
While some studies have linked chronic cannabis use to changes in the brain’s structure and function, outcomes vary depending, in part, on how and when people use the substance. People who begin using cannabis during adolescence, while the brain is still developing, may be particularly vulnerable to brain changes. The potency of the products they use and how often they use them matter, too.
Participants in the research, who obtained medical cannabis cards at the outset of the study, tended to choose lower potency products and use them less than daily. This may be why the researchers’ analysis—which focused on the brain activity associated with three kinds of cognitive processes—showed no changes after a year of use.
“For most older adults, occasional cannabis will not dramatically affect brain activation,” says Harvard neuroscientist Jodi Gilman, who led the study. “However, there are some individuals who may be vulnerable to negative effects of cannabis on cognitive function, particularly those using higher potency products more frequently.”
Gilman cautions that in another study of the same medical cannabis users, her team found that the drug failed to alleviate patients’ pain, depression, or anxiety. “So it didn’t help their symptoms—but it wasn’t associated with significant changes in brain activation,” she says. She also cautioned that some adults in the study did develop problems with cannabis use, including cannabis use disorder.
Medical cannabis programs are currently established in 38 U.S. states and Washington, D.C., increasing access to a substance that many people hope might help them relieve distressing medical symptoms. But little is known about how this type of cannabis use affects neural circuits in the brain. “Cannabis has been legalized through ballot initiatives and by legislatures. Dispensary cannabis has not been tested through large, randomized, double-blind clinical trials,” Gilman says. With McGovern Principal Research Scientist Satrajit Ghosh and MD-PhD student Debbie Burdinski, she set out to see what neuroimaging data would reveal about the impacts of this type of cannabis use.
Participants in their study were all adults seeking relief from depression, anxiety, pain, or insomnia who, prior to obtaining their medical cannabis cards, had never used cannabis at high frequencies. The researchers wanted their study to reflect the ways people really use cannabis, so participants were free choose which types of products they used, as well as how much and how often. “We told people, “Get what you want, use it you as you wish, and we’re going to look at how it may affect the brain,” Gilman explains.
Participants reported using a variety of products, but generally, they tended to choose low-potency products. Their frequency of use also varied, from less than once a month to once or more each day. Fewer than 20 percent of participants were daily users.
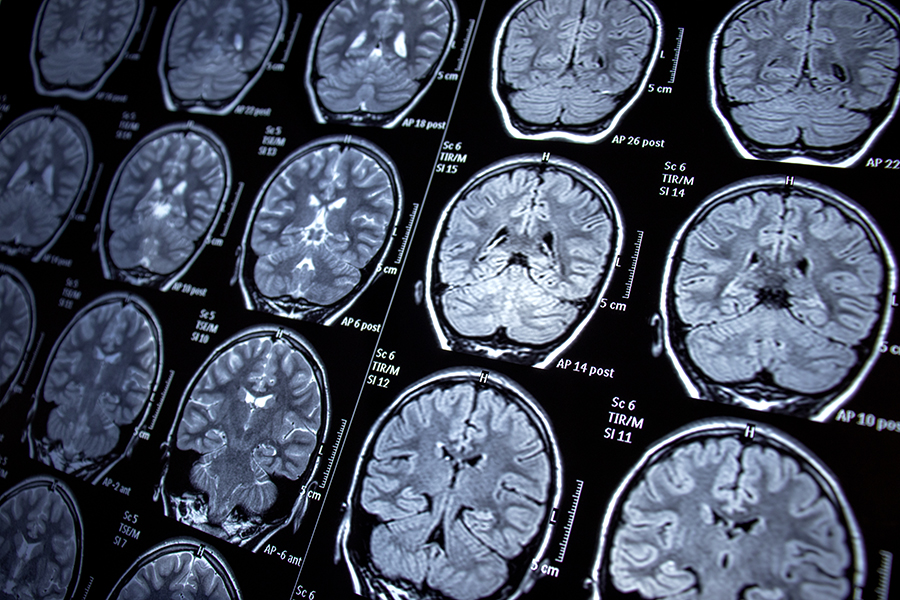
At the start of the study and again one year later, the research team used functional MRI scans to watch what happened in the brain while participants used three key cognitive skills: working memory, inhibitory control, and reward processing. The activity revealed on the scans showed the researchers which parts of the brain were working to perform these tasks.
Alterations in activity patterns could indicate changes in brains function. But in the 54 participants who underwent both brain scans, Gilman, Ghosh, and Burdinski found that after one year of cannabis use, brain activity during these three cognitive tasks was unchanged. Burdinski notes that many facets of cognition were not followed in the study, so some changes to brain activity could have occurred without being evident in the team’s data.
The researchers acknowledge that their study cohort, whose members were mostly female, middle-aged, and well educated, was less diverse than the population of people who use cannabis for medical symptoms. In fact, Gilman says, groups that are most vulnerable to negative consequences of cannabis may not have been well represented in the study, and it’s possible that a study of a different subgroup would have found different results.
Ghosh points out that there is still a lot to learn about the impact of cannabis, and larger studies are needed to understand its effects on the brain, including how it impacts different populations. For some individuals, he stresses, its use can have severe, debilitating effects, including symptoms of psychosis, delusions, or cannabinoid hyperemesis syndrome.
Larger studies are needed to understand cannabis’s effects on the brain and how it impacts different populations, Ghosh says. “Science can help us understand how we should be thinking about the impact of various substances or various interventions on the brain, instead of just anecdotal considerations of how they work,” he says. “Maybe there are people for whom there are changes. Now we can start teasing apart those details.”
Paper; "Year-Long Cannabis Use for Medical Symptoms and Brain Activation During Cognitive Processes"