The National Academy of Medicine recently announced the election of more than 90 members during its annual meeting, including MIT faculty members Matthew Vander Heiden and Fan Wang, along with five MIT alumni.
Election to the National Academy of Medicine (NAM) is considered one of the highest honors in the fields of health and medicine and recognizes individuals who have demonstrated outstanding professional achievement and commitment to service.
Matthew Vander Heiden is the director of the Koch Institute for Integrative Cancer Research at MIT, a Lester Wolfe Professor of Molecular Biology, and a member of the Broad Institute of MIT and Harvard. His research explores how cancer cells reprogram their metabolism to fuel tumor growth and has provided key insights into metabolic pathways that support cancer progression, with implications for developing new therapeutic strategies. The National Academy of Medicine recognized Vander Heiden for his contributions to “the development of approved therapies for cancer and anemia” and his role as a “thought leader in understanding metabolic phenotypes and their relations to disease pathogenesis.”
Vander Heiden earned his MD and PhD from the University of Chicago and completed his clinical training in internal medicine and medical oncology at the Brigham and Women’s Hospital and the Dana-Farber Cancer Institute. After postdoctoral research at Harvard Medical School, Vander Heiden joined the faculty of the MIT Department of Biology and the Koch Institute in 2010. He is also a practicing oncologist and instructor in medicine at Dana-Farber Cancer Institute and Harvard Medical School.
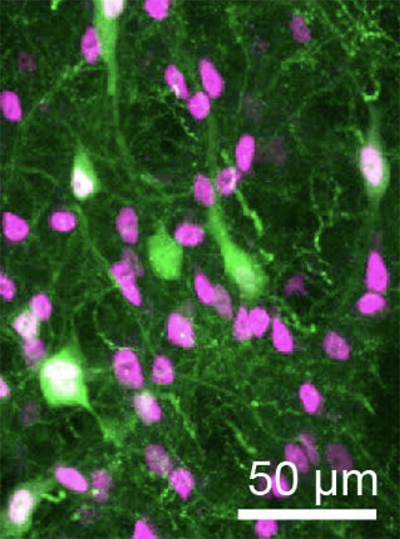
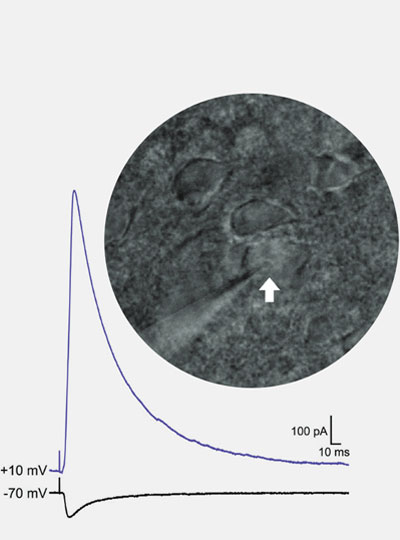
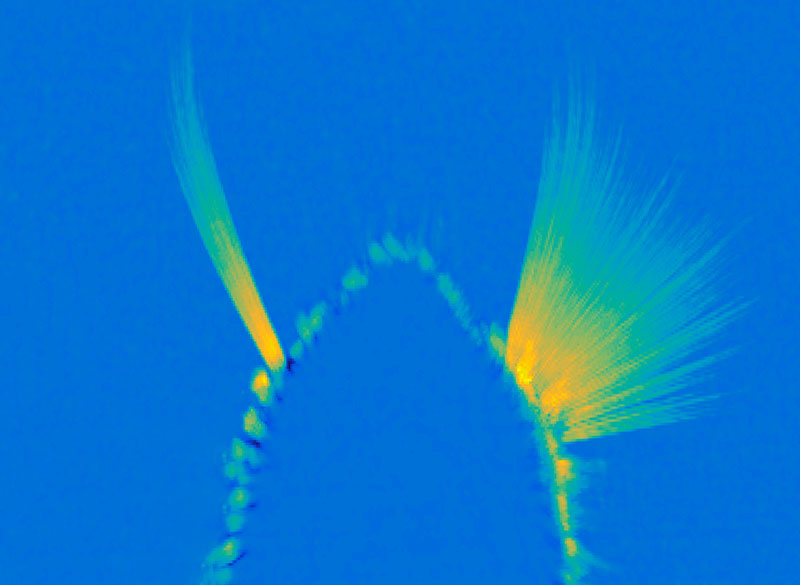
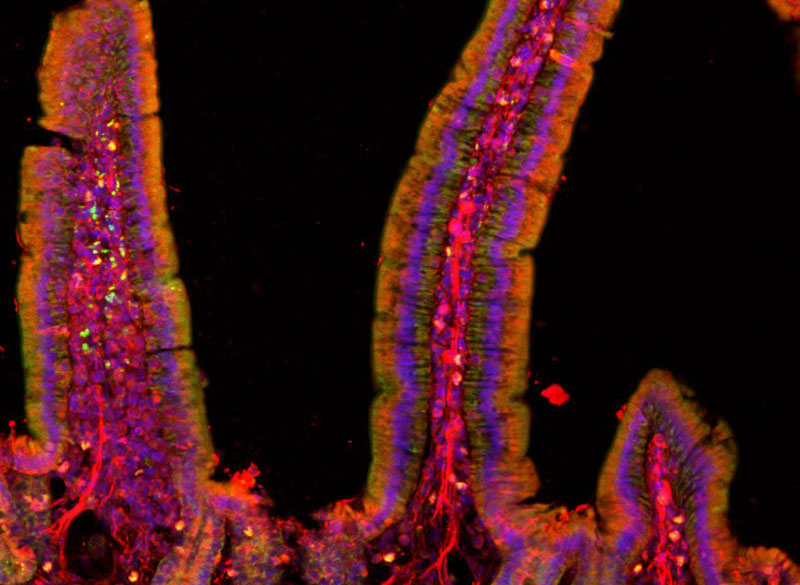
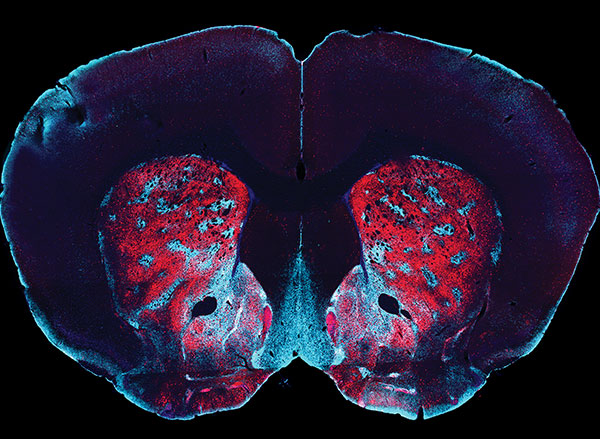
Fan Wang is a professor of brain and cognitive sciences, an investigator at the McGovern Institute, and director of the K. Lisa Yang and Hock E. Tan Center for Molecular Therapeutics at MIT. Wang’s research focuses on the neural circuits governing the bidirectional interactions between the brain and body. She is specifically interested in the circuits that control the sensory and emotional aspects of pain and addiction, as well as the sensory and motor circuits that work together to execute behaviors such as eating, drinking, and moving. The National Academy of Medicine has recognized her body of work for “providing the foundational knowledge to develop new therapies to treat chronic pain and movement disorders.”
Before coming to MIT in 2021, Wang obtained her PhD from Columbia University and received her postdoctoral training at the University of California at San Francisco and Stanford University. She became a faculty member at Duke University in 2003 and was later appointed the Morris N. Broad Professor of Neurobiology. Wang is also a member of the American Academy of Arts and Sciences and she continues to make important contributions to the neural mechanisms underlying general anesthesia, pain perception, and movement control.
MIT alumni who were elected to the NAM for 2024 include:
- Leemore Dafny PhD ’01 (Economics);
- David Huang ’85 MS ’89 (Electrical Engineering and Computer Science) PhD ’93 Medical Engineering and Medical Physics);
- Nola M. Hylton ’79 (Chemical Engineering);
- Mark R. Prausnitz PhD ’94 (Chemical Engineering); and
- Konstantina M. Stankovic ’92 (Biology and Physics) PhD ’98 (Speech and Hearing Bioscience and Technology)
Established originally as the Institute of Medicine in 1970 by the National Academy of Sciences, the National Academy of Medicine addresses critical issues in health, science, medicine, and related policy and inspires positive actions across sectors.
“This class of new members represents the most exceptional researchers and leaders in health and medicine, who have made significant breakthroughs, led the response to major public health challenges, and advanced health equity,” said National Academy of Medicine President Victor J. Dzau. “Their expertise will be necessary to supporting NAM’s work to address the pressing health and scientific challenges we face today.”