McGovern researchers are finding neural markers that could help improve treatment for psychiatric patients.
Ten years ago, Jim and Pat Poitras committed $20M to the McGovern Institute to establish the Poitras Center for Affective Disorders Research. The Poitras family had been longtime supporters of MIT, and because they had seen mental illness in their own family, they decided to support an ambitious new program at the McGovern Institute, with the goal of understanding the fundamental biological basis of depression, bipolar disorder, schizophrenia and other major psychiatric disorders.
The gift came at an opportune time, as the field was entering a new phase of discovery, with rapid advances in psychiatric genomics and brain imaging, and with the emergence of new technologies for genome editing and for the development of animal models. Over the past ten years, the Poitras Center has supported work in each of these areas, including Feng Zhang’s work on CRISPR-based genome editing, and Guoping Feng’s work on animal models for autism, schizophrenia and other psychiatric disorders.
This reflects a long-term strategy, says Robert Desimone, director of the McGovern Institute who oversees the Poitras Center. “But we must not lose sight of the overall goal, which is to benefit human patients. Insights from animal models and genomic medicine have the potential to transform the treatments of the future, but we are also interested in the nearer term, and in what we can do right now.”
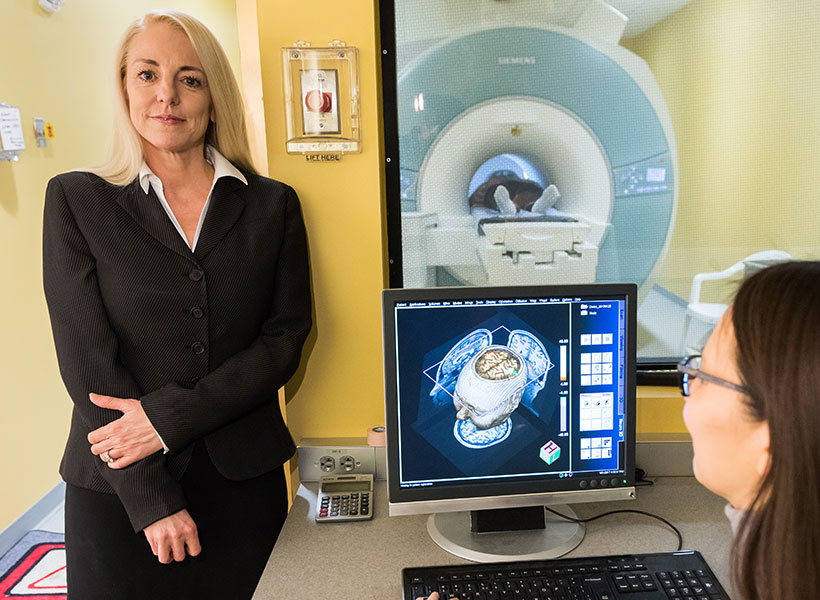
One area where technology can have a near-term impact is human brain imaging, and in collaboration with clinical researchers at McLean Hospital, Massachusetts General Hospital and other institutions, the Poitras Center has supported an ambitious program to bring human neuroimaging closer to the clinic.
Discovering psychiatry’s crystal ball
A fundamental problem in psychiatry is that there are no biological markers for diagnosing mental illness or for indicating how best to treat it. Treatment decisions are based entirely on symptoms, and doctors and their patients will typically try one treatment, then if it does not work, try another, and perhaps another. The success rates for the first treatments are often less than 50%, and finding what works for an individual patient often means a long and painful process of trial and error.
“Someday, a person will be able to go to a hospital, get a brain scan, charge it to their insurance, and know that it helped the doctor select the best treatment,” says Satra Ghosh.
McGovern research scientist Susan Whitfield-Gabrieli and her colleagues are hoping to change this picture, with the help of brain imaging. Their findings suggest that brain scans can hold valuable information for psychiatrists and their patients. “We need a paradigm shift in how we use imaging. It can be used for more than research,” says Whitfield-Gabrieli, who is a member of McGovern Investigator John Gabrieli’s lab. “It would be a really big boost to be able use it to personalize psychiatric medicine.”
One of Whitfield-Gabrieli’s goals is to find markers that can predict which treatments will work for which patients. Another is to find markers that can predict the likely risk of disease in the future, allowing doctors to intervene before symptoms first develop. All of these markers need further validation before they are ready for the clinic, but they have the potential to meet a dire need to improve treatment for psychiatric disease.
A brain at rest
For Whitfield-Gabrieli, who both collaborates with and is married to Gabrieli, that paradigm shift began when she started to study the resting brain using functional magnetic resonance imaging (fMRI). Most brain imaging studies require the subject to perform a mental task in the scanner, but these are time-consuming and often hard to replicate in a clinical setting.In contrast, resting state imaging requires no task. The subject simply lies in the scanner and lets the mind wander. The patterns of activity can reveal functional connections within the brain, and are reliably consistent from study to study.
Whitfield-Gabrieli thought resting state scanning had the potential to help patients because it is simple and easy to perform.
“Even a 5-minute scan can contain useful information that could help people,” says Satrajit Ghosh, a principal research scientist in the Gabrieli lab who works closely with Whitfield-Gabrieli.
Whitfield-Gabrieli and her clinical collaborator Larry Seidman at Harvard Medical School decided to study resting state activity in patients with schizophrenia. They found a pattern of activity strikingly different from that of typical brains. The patients showed unusually strong activity in a set of interconnected brain regions known as the default mode network, which is typically activated during introspection. It is normally suppressed when a person attends to the outside world, but schizophrenia patients failed to show this suppression.
“The patient isn’t able to toggle between internal processing and external processing the way a typical individual can,” says Whitfield-Gabrieli, whose work is supported by the Poitras Center for Affective Disorders Research.
Since then, the team has observed similar disturbances in the default network in other disorders, including depression, anxiety, bipolar disorder, and ADHD. “We knew we were onto something interesting,” says Whitfield-Gabrieli. “But we kept coming back to the question: how can brain imaging help patients?”
fMRI on patients
Many imaging studies aim to understand the biological basis of disease and ultimately to guide the development of new drugs or other treatments. But this is a long-term goal, and Whitfield-Gabrieli wanted to find ways that brain imaging could have a more immediate impact. So she and Ghosh decided to use fMRI to look at differences among individual patients, and to focus on differences in how they responded to treatment.
“It gave us something objective to measure,” explains Ghosh. “Someone goes through a treatment, and they either get better or they don’t.” The project also had appeal for Ghosh because it was an opportunity for him to use his expertise in machine learning and other computational tools to build systems-level models of the brain.
For the first study, the team decided to focus on social anxiety disorder (SAD), which is typically treated with either prescription drugs or cognitive behavioral therapy (CBT). Both are moderately effective, but many patients do not respond to the first treatment they try.
The team began with a small study to test whether scans performed before the onset of treatment could predict who would respond best to the treatment. Working with Stefan Hofmann, a clinical psychologist at Boston University, they scanned 38 SAD patients before they began a 12-week course of CBT. At the end of their treatment, the patients were evaluated for clinical improvement, and the researchers examined the scans for patterns of activity that correlated with the improvement. The results were very encouraging; it turned out that predictions based on scan data were 5-fold better than the existing methods based on severity of symptoms at the time of diagnosis.
The researchers then turned to another condition, ADHD, which presents a similar clinical challenge, in that commonly used drugs—such as Adderall or Ritalin—work well, but not for everyone. So the McGovern team began a collaboration with psychiatrist Joseph Biederman, Chief of Clinical and Research Programs in Pediatric Psychopharmacology and Adult ADHD
at Massachusetts General Hospital, on a similar study, looking for markers of treatment response.
The study is still ongoing, and it will be some time before results emerge, but the researchers are optimistic. “If we could predict who would respond to which treatment and avoid months of trial and error, it would be totally transformative for ADHD,” says Biederman.
Another goal is to predict in advance who is likely to develop a given disease in the future. The researchers have scanned children who have close relatives with schizophrenia or depression, and who are therefore at increased risk of developing these disorders themselves. Surprisingly, the children show patterns of resting state connectivity similar to those of patients.
“I was really intrigued by this,” says Whitfield-Gabrieli. “Even though these children are not sick, they have the same profile as adults who are.”
Whitfield-Gabrieli and Seidman are now expanding their study through a collaboration with clinical researchers at the Shanghai Mental Institute in China, who plan to image and then follow 225 people who are showing early risk signs for schizophrenia. They hope to find markers that predict who will develop the disease and who will not.
“While there are no drugs available to prevent schizophrenia, it may be possible to reduce the risk or severity of the disorder through CBT, or through interventions that reduce stress and improve sleep and well-being,” says Whitfield-Gabrieli. “One likely key to success is early identification of those at highest risk. If we could diagnose early, we could do early interventions
and potentially prevent disorders.”
From association to prediction
The search for predictive markers represents a departure from traditional psychiatric imaging studies, in which a group of patients is compared with a control group of healthy subjects. Studies of this type can reveal average differences between the groups, which may provide clues to the underlying biology of the disease. But they don’t provide information about individual patients, and so they have not been incorporated into clinical practice.
The difference is critical for clinicians, says Biederman. “I treat individuals, not groups. To bring predictive scans to the clinic, we need to be sure the individual scan is informative for the person you are treating.”
To develop these predictions, Whitfield-Gabrieli and Ghosh must first use sophisticated computational methods such as ‘deep learning’ to identify patterns in their data and to build models that relate the patterns to the clinical outcomes. They must then show that these models can generalize beyond the original study population—for example, that predictions based on patients from Boston can be applied to patients from Shanghai. The eventual goal is a model that can analyze a previously unseen brain scan from any individual, and predict with high confidence whether that person will (for example) develop schizophrenia or respond successfully to a particular therapy.
Achieving this will be challenging, because it will require scanning and following large numbers of subjects from diverse demographic groups—thousands of people, not just tens or hundreds
as in most clinical studies. Collaborations with large hospitals, such as the one in Shanghai, can help. Whitfield-Gabrieli has also received funding to collect imaging, clinical, and behavioral
data from over 200 adolescents with depression and anxiety, as part of the National Institutes of Health’s Human Connectome effort. These data, collected in collaboration with clinicians at
McLean Hospital, MGH and Boston University, will be available not only for the Gabrieli team, but for researchers anywhere to analyze. This is important, because no one team or center can
do it alone, says Ghosh. “Data must be collected by many and shared by all.”
The ultimate goal is to study as many patients as possible now so that the tools can help many more later. “Someday, a person will be able to go to a hospital, get a brain scan, charge it to their insurance, and know that it helped the doctor select the best treatment,” says Ghosh. “We’re still far away from that. But that is what we want to work towards.”