A new atlas developed by researchers at MIT’s McGovern Institute and Harvard Medical School catalogs a diverse array of brain cells throughout the marmoset brain. The atlas helps establish marmosets—small monkeys whose brains share many functional and structural features with the human brain—as a valuable model for neuroscience research.
Data from more than two million brain cells are included in the atlas, which spans 18 regions of the marmoset brain. A research team led by Guoping Feng, associate director of the McGovern Institute and member of the Broad Institute of Harvard and MIT, Harvard biologist and member of the Broad Institute of Harvard and MIT Steven McCarroll, and Princeton neurobiologist Fenna Krienen classified each cell according to its particular pattern of genetic activity, providing an important reference for studies of the marmoset brain. The team’s analysis, reported October 13, 2023, in the journal Science Advances, also reveals the profound influence of a cell’s developmental origin on its identity in the primate brain.
Cellular diversity
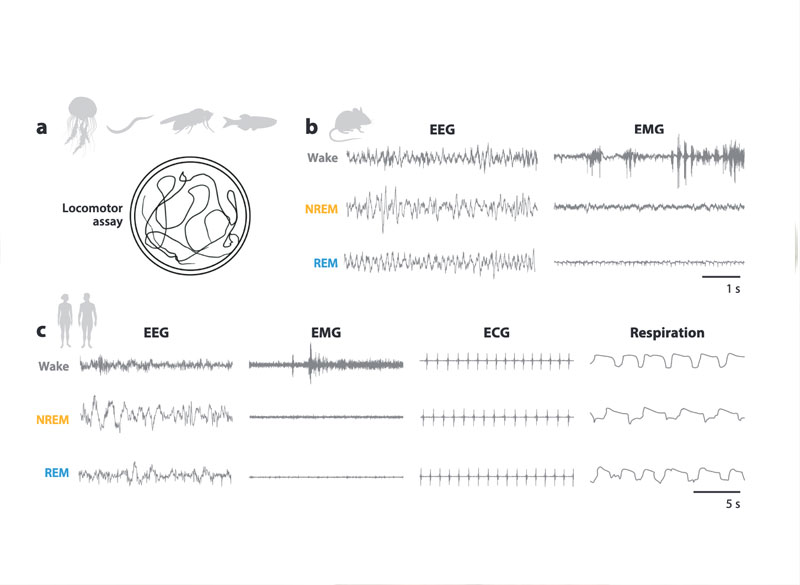
Brains are made up of a tremendous diversity of cells. Neurons with dramatically different gene expression, shapes, and activities work together to process information and drive behavior, supported by an assortment of immune cells and other cell types. Scientists have only recently begun to catalog this cellular diversity—first in mice, and now in primates.
The marmoset is a quick-breeding monkey whose small brain has many of features similar to those that enable higher cognitive processes in humans. Feng says neuroscientists have begun turning to marmosets as a research model in recent years because new gene editing technology has made it easier to modify the animal’s DNA, so scientists can now study the genetic factors that shape marmosets’ brains and behavior. Feng, McCarroll, Krienen and others hope these animals will offer insights into how primate brains handle complex decision-making, social interactions, and other higher brain functions that are difficult to study in mice. Likewise, Feng says, the monkeys will help scientists investigate the impact of genetic mutations associated with brain disorders and explore potential therapeutic strategies.
To make marmosets a practical model for neuroscience, scientists need to understand the fundamental composition of their brains. Feng and McCarroll’s team have begun that characterization with their cell census, which was supported by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative’s Cell Census Network (BICCN), as part a larger effort to map cellular features in the brains of mice, non-human primates, and humans. It is an essential first step in the creation of a comprehensive atlas charting the molecular, anatomical, and functional features of cells in the marmoset brain.
“Hopefully, when the BRAIN Initiative is complete, we will have a very complete map of these cells: where they are located, their abundance, their functional properties,” says Feng. “This not only gives you knowledge of the normal brain, but you can also look at what aspects change in diseases of the brain. So it’s a really powerful database.”
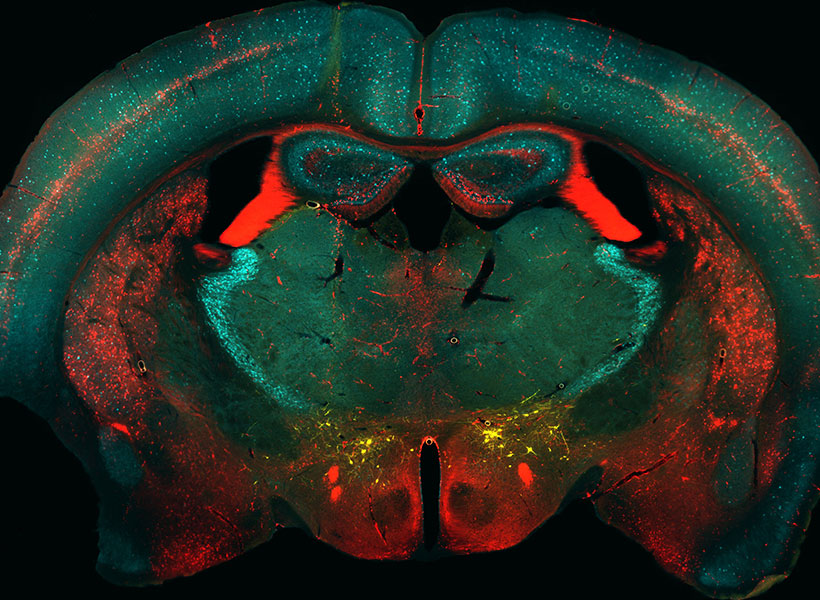
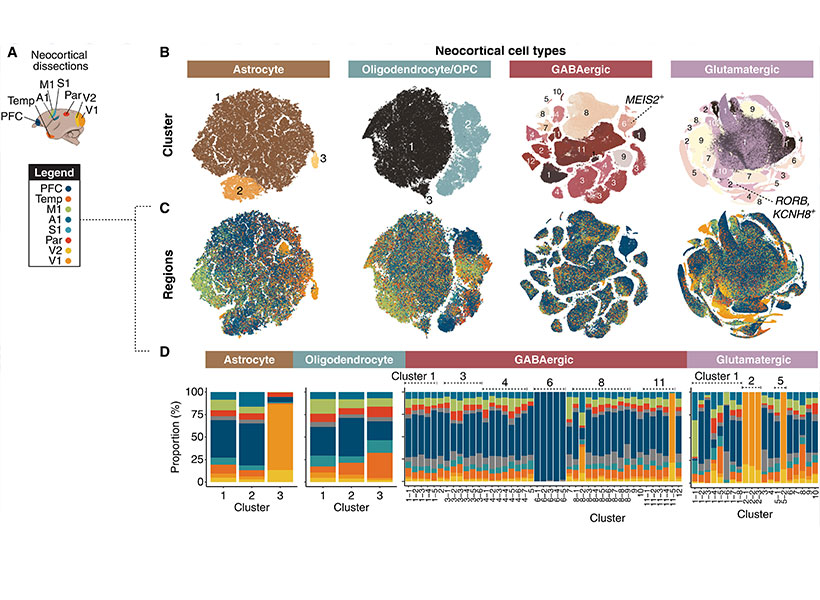
To catalog the diversity of cells in the marmoset brain, the researchers undertook an expansive analysis of the molecular contents of 2.4 million brain cells from adult marmosets. For each of these cells, they analyzed the complete set of RNA copies of its genes that the cell had produced, known as the cell’s transcriptome. Because the transcriptome captures patterns of genetic activity inside a cell, it is an indication of the cell’s function and can be used to assess cellular identity.
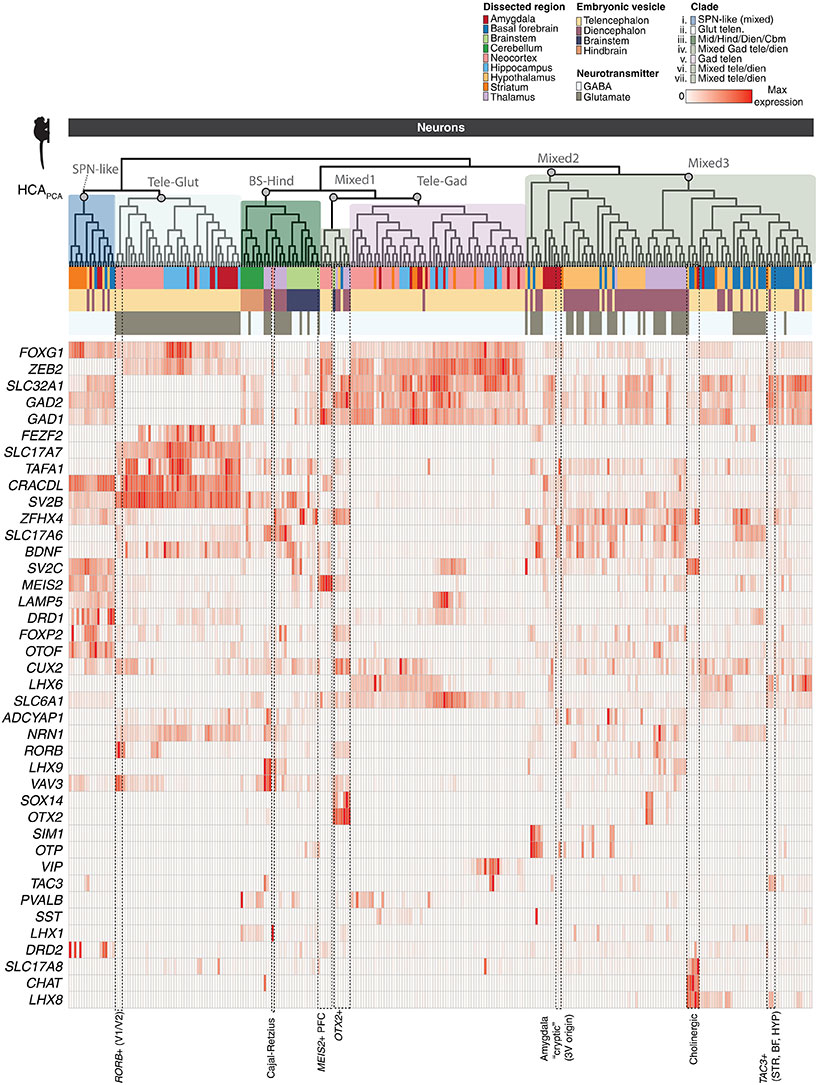
The team’s analysis is one of the first to compare patterns of gene activity in cells from disparate regions of the marmoset brain. Doing so yielded surprising insights into the factors that shape brain cells’ transcriptomic identities. “What we found is that the cell’s transcriptome contains breadcrumbs that link back to the developmental origin of that cell type,” says Krienen, who led the cellular census as a postdoctoral researcher in McCarroll’s lab. That suggests that comparing cells’ transcriptomes can help scientists figure out how primate brains are assembled, which might lead to insights into neurodevelopmental disorders, she says.
The team also learned that a cell’s location in the brain was critical to shaping its transcriptomic identity. For example, Krienen says, “it turns out that an inhibitory neuron in the cortex doesn’t look very anything like an inhibitory neuron in the thalamus, probably because they have distinct embryonic origins.”
Expanding the cell census
This new picture of cellular diversity in the marmoset brain will help researchers understand how genetic perturbations affect different brain cells and interpret the results of future experiments. Importantly, Krienen says, it could help researchers pinpoint exactly which cells are affected in brain disorders, and how the effects of a disease might localize to specific brain regions.
Krienen, McCarroll, and Feng went beyond their initial survey of cellular diversity with analyses of specific subsets of cells, charting the spatial distribution of interneurons in a key region of the prefrontal cortex and visualizing the shapes of several molecularly-defined cell types. Now, they have begun expanding their cell census beyond the 18 brain structures represented in the reported work. As part of the BRAIN Initiative’s Brain Cell Atlas Network (BICAN), the team will profile cells throughout the entire adult marmoset brain, including multiple data types in their analysis. Building on cell census data, NIH BRAIN Initiative has also launched BRAIN CONNECTS projects to map cellular connectivity in the brain.
This work was supported by the National Institutes of Health, the National Science Foundation, MathWorks, MIT, Harvard Medical School, the Broad Institute’s Stanley Center for Psychiatric Research, the Hock E. Tan and K. Lisa Yang Center for Autism Research at MIT, the Poitras Center for Psychiatric Disorders Research at MIT, and the McGovern Institute for Brain Research at MIT.