General anesthesia is medication that suppresses pain and renders patients unconscious during surgery, but whether pain suppression is simply a side effect of loss of consciousness has been unclear. Fan Wang and colleagues have now identified the circuits linked to pain suppression under anesthesia in mouse models, showing that this effect is separable from the unconscious state itself.
“Existing literature suggests that the brain may contain a switch that can turn off pain perception,” explains Fan Wang, a professor at Duke University and lead author of the study. “I had always wanted to find this switch, and it occurred to me that general anesthetics may activate this switch to produce analgesia.”
Wang, who will join the McGovern Institute in January 2021, set out to test this idea with her student, Thuy Hua, and postdoc, Bin Chen.
Pain suppressor
Loss of pain, or analgesia, is an important property of anesthetics that helps to make surgical and invasive medical procedures humane and bearable. In spite of their long use in the medical world, there is still very little understanding of how anesthetics work. It has generally been assumed that a side effect of loss of consciousness is analgesia, but several recent observations have brought this idea into question, and suggest that changes in consciousness might be separable from pain suppression.
A key clue that analgesia is separable from general anesthesia comes from the accounts of patients that regain consciousness during surgery. After surgery, these patients can recount conversations between staff or events that occurred in the operating room, despite not feeling any pain. In addition, some general anesthetics, such as ketamine, can be deployed at low concentrations for pain suppression without loss of consciousness.
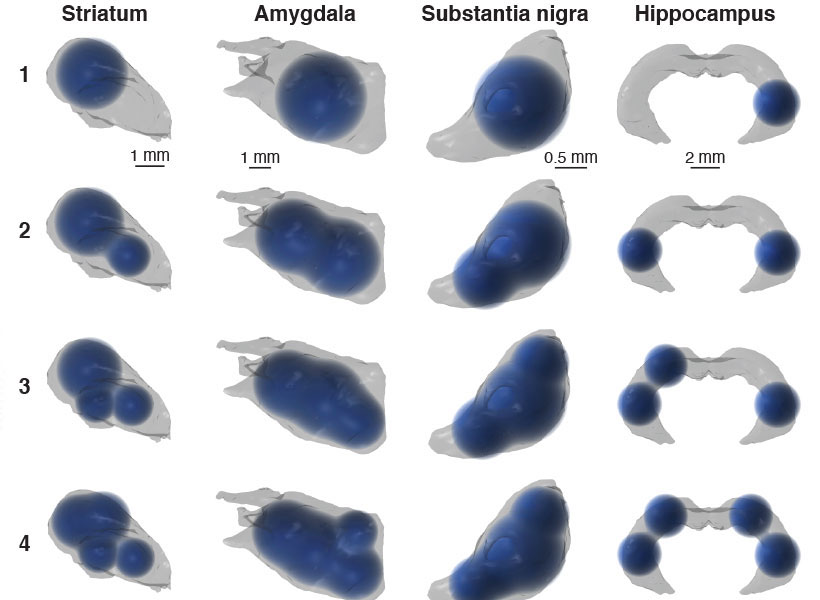
Following up on these leads, Wang and colleagues set out to uncover which neural circuits might be involved in suppressing pain during exposure to general anesthetics. Using CANE, a procedure developed by Wang that can detect which neurons activate in response to an event, Wang discovered a new population of GABAergic neurons activated by general anesthetic in the mouse central amygdala.
These neurons become activated in response to different anesthetics, including ketamine, dexmedetomidine, and isoflurane. Using optogenetics to manipulate the activity state of these neurons, Wang and her lab found that they led to marked changes in behavioral responses to painful stimuli.
“The first time we used optogenetics to turn on these cells, a mouse that was in the middle of taking care of an injury simply stopped and started walked around with no sign of pain,” Wang explains.
Specifically, activating these cells blocks pain in multiple models and tests, whereas inhibiting these neurons rendered mice aversive to gentle touch — suggesting that they are involved in a newly uncovered central pain circuit.
The study has implications for both anesthesia and pain. It shows that general anesthetics have complex, multi-faceted effects and that the brain may contain a central pain suppression system.
“We want to figure out how diverse general anesthetics activate these neurons,” explains Wang. “That way we can find compounds that can specifically activate these pain-suppressing neurons without sedation. We’re now also testing whether placebo analgesia works by activating these same central neurons.”
The study also has implications for addiction as it may point to an alternative system for central pain suppression that could be a target of drugs that do not have the devastating side effects of opioids.